Telehealth in rural areas provides a dose of innovation
As an educator and tech strategist, I have the privilege of working with many of the world’s leading technology companies. AT&T Business, the sponsor of this post, is one. The opinions expressed in this post may or may not reflect the views of any company I work with. My goal is to make technology more accessible and beneficial for all. Having served on the board of directors of a university hospital for several years, I have an abiding interest in healthcare accessibility.
A "digital divide" between those with access to high-speed internet and those without is growing in the United States, according to a recent report by the U.S. Congressional Research Service1. That divide is contributing to a widening divide in access to healthcare.
Telemedicine and telehealth importance for rural health
Telemedicine and telehealth offer an opportunity to make healthcare more accessible to rural and underserved communities—if reliable, high-speed internet connectivity can likewise become more accessible to these communities.
The terms "telemedicine" and "telehealth" are often used interchangeably, but there is a subtle difference between the two, according to the U.S. Office of the National Coordinator for Health Information Technology (ONC):
While telemedicine refers specifically to remote clinical services, telehealth can refer to remote non-clinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
The ONC observes that telemedicine empowers patients in rural communities to receive quality medical care in their communities without having to travel long distances, often meaning the difference between care and no care.
More than 46 million Americans, or 14 percent of the U.S. population, live in rural areas2—sparsely populated and often distant from urban centers and medical facilities.
According to the U.S. Center for Disease Control, "People who live in rural areas of the United States are more likely than urban residents to die prematurely from five of the leading causes of death: heart disease, cancer, unintentional injury, chronic lower respiratory disease, and stroke.” 3
The ONC highlights the importance of "telecommunications technologies" in rural settings:
"Imagine a rural primary care provider (PCP) needs to refer a patient to a Stroke Specialist in an area where no such specialists practice. With telehealth, the PCP may be able to leverage telecommunications technologies to connect the patient with a specialist at a remote site instead of asking the patient to travel to another community to obtain care." With access to telemedicine, specialized care becomes more accessible for rural residents, improving patient outcomes.
Telehealth and rural healthcare workforce development and retention
“Rural healthcare workers are often reluctant to leave their homes or place of employment for training and education due to travel challenges, coverage in staffing, family commitments, and costs. Online and telehealth training programs can provide accessible training for current and future healthcare professionals,” notes the Rural Health Information Hub, a US, federally-funded clearinghouse on rural health issues4.
Innovation of virtual healthcare solutions in telemedicine, especially in rural communities, is improving patient outcomes as noted in a study, Telehealth Interventions and Outcomes Across Rural Communities in the United States, highlighted by the National Institute of Health5. A series of studies cited the benefits of "decreased direct and indirect costs to the patient (travel cost and time) and health care service provider (staffing), lower onsite health care resource utilization, improved physician recruitment and retention, improved access to care, and increased education and training of patients and health care professionals."
With virtual reality learning platforms, telehealth is entering the metaverse
Purdue School of Nursing uses virtual reality to make healthcare training more accessible and standardized. In January 2022 they announced that “Having found virtual reality learning to be successful for its students, the Purdue University Global School of Nursing now is making its immersive learning technology available to other organizations.” Located in West Fayetteville, Indiana. This is in collaboration with InciteVR—“a company that specializes in the production of immersive learning products for higher education and professional training.” Purdue University calls the use of “clinical immersives”, virtual reality (VR), a ‘game changer’ for health care students and practitioners6.
“Cloud-based delivery (of immersive nursing education) allows for ‘anywhere, anytime' access. The availability to practice is nearly unlimited,” said associate dean of graduate nursing at Purdue Global School of Nursing, Michele McMahon7.
Training in VR helps address workforce shortages in healthcare
Purdue notes that “The use of VR offers expanded access to critical education, focusing on the hard and soft skills necessary in health care practice with increased flexibility for students to learn on their own schedule. In this way, incorporating VR in clinical education helps to combat the shortage and constraints felt across numerous disciplines within healthcare.”
This innovative VR training offers keen advantages to healthcare providers in rural communities who would otherwise need to travel long distances to learn new skills or hone existing ones.
Telehealth platforms offer secure, seamless healthcare provider/patient connectivity
For communities and healthcare providers, AT&T Business, a telehealth leader, streamlines the transformation to telehealth and telemedicine with "end-to-end, ready-to-use," "virtual care platforms," improving patient access, affordability, and convenience.
Remote patient monitoring (RPM) through the platform lets healthcare professionals track patient vitals and health data remotely, in real time, while adhering to strict HIPAA security and privacy requirements. Healthcare professionals can message patients instantly and securely from the digital portal with two-way video and audio calls with photo sharing.
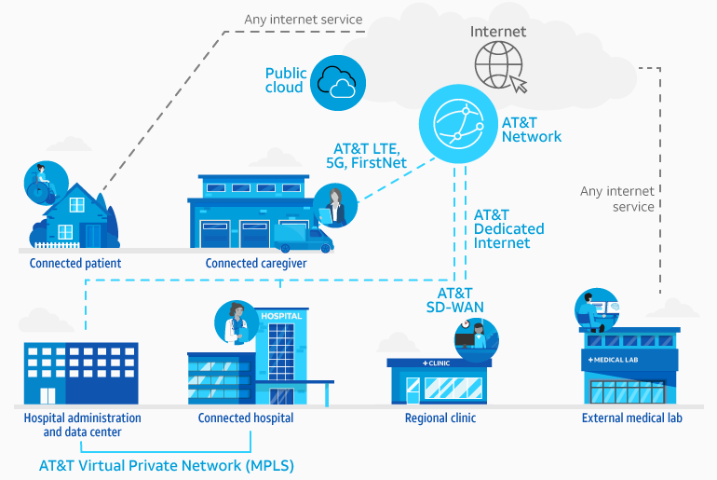
Cybersecurity precautions and protections are key to any telehealth initiative. Successful, sustainable healthcare digital platforms require highly-secure, encrypted communications and devices that guard against mobile-based attacks.
In addition to remote patient monitoring, telehealth platforms can be used to send patients "gentle reminders of doctors’ appointments, prescription information, or vital signs readings," enhancing patient care and safety, reducing missed appointments, and improving medication compliance, all leading to cost savings and improved patient care outcomes.
Closing the digital and healthcare divide
"While the number of new broadband subscribers continues to grow, studies and data indicate that the rate of broadband deployment in urban/suburban and high-income areas is outpacing deployment in rural and low-income areas," noted the Congressional research service in its 2021 report, The Digital Divide: What Is It, Where Is It, and Federal Assistance Programs.
In October of 2021, the U.S. Department of Agriculture (USDA) announced a $1.15 billion dollar initiative to accelerate access to high-speed internet "for millions of rural Americans nationwide," as well as for tribal lands and "socially vulnerable communities." Telehealth and telemedicine are central to that initiative, with a focus on helping to provide "access to specialized health care". With this initiative, telehealth and telemedicine should take a giant leap forward, providing healthcare accessibility to record numbers of people8.
For more information on the technologies fueling Healthcare or contact your AT&T Business representative.
1 “The digital divide: What Is It, Where is it, and Federal Assistance Programs”. Congressional Research Service (March 2021).
2 Elizabeth A. Dobis, Thomas P. Krumel, Jr., John Cromartie, Kelsey L. Conley, Austin Sanders, and Ruben Ortiz, ”Rural America at a Glance: 2021 Edition,” U.S. Department of Agriculture, November 2021.
3 “Public Health Research in Rural Communities,” U.S. Centers for Disease Control, Accessed November 10, 2022.
4 “About the Rural Health Information Hub,” Rural Health Information Hub, Accessed November 10, 2022, https://www.ruralhealthinfo.org/about.
5 Rita Kukafka, “Telehealth Interventions and Outcomes Across Rural Communities in the Uniter States: Narrative Review,” National Library of Medicine, August 26, 2021), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8430850/.
6 “Introducing Clinic Immersives by Purdue University Global: ‘A Game Changer’ for Health Care Students and Practitioners,” Purdue University News, January 12 2022, https://www.purdue.edu/newsroom/releases/2022/Q1/introducing-clinic-immersives-by-purdue-university-global-a-game-changer-for-health-care-students-and-practitioners.html.
7 “The Future of Virtual Reality in Nursing Education,” Purdue University Global, January 11, 2021.
8 USDA to Make Up to $1.15 Billion Available to Help People Living in Rural Communities Access High-Speed Internet. U.S. Department of Agriculture (Oct 2021).




Share
Share this with others